Introduction
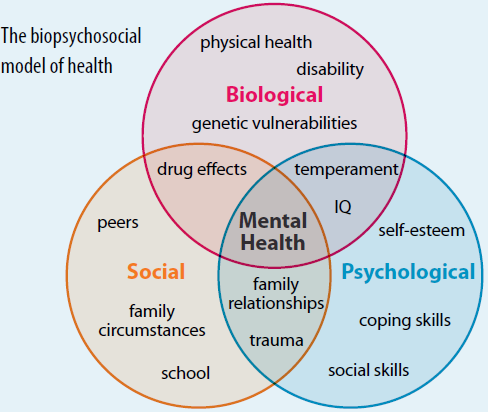
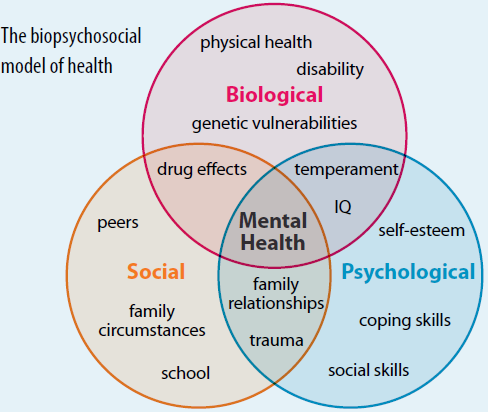
The Biopsychosocial model was first conceptualised by George Engel in 1977, suggesting that to understand a person’s medical condition it is not simply the biological factors to consider, but also the psychological and social factors [1].
- Bio (physiological pathology) what appears to be the actual physical problem?
- Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution) How is it making you feel? What are the emotions tied up with your situation?
- Social (socio-economical, socio-environmental, and cultural factors such as work issues, family circumstances and benefits/economics). How is it impacting on your life or how are those around you impacting on your recovery and beliefs about recovery?
This model is commonly used when talking about chronic pain with the view that the pain is a psychophysiological behaviour pattern that cannot be categorised into biological, psychological, or social factors alone, or as is often said; ‘pain is multifactorial’. There are suggestions that physiotherapy should integrate psychological treatment to address all components comprising the experience of chronic pain.
Physiotherapists must try to understand how biopsychosocial factors interact in patients with pain to explain the perpetuation of this condition and use it as a basis for planning the intervention program. The evidence has suggested a clinical biopsychosocial assessment for the physiotherapeutic management of patients with chronic pain in order to understand and explain the predominant mechanism of pain and psychosocial factors that may or may not be modified for the patient to improve their condition.
So essentially the biopsychosocial approach attempts to consider all of the factors that are contributing to the patients situation. For example if you injure a knee and cannot drive to work for a prolonged period that then effects your pay. You have a partner with two young children who are relying on those wages to live, the potential impact on you and your recovery could be far more than the injury itself.
Clinical Contribution
- The use of the biopsychosocial model as a clinical practice guide in physiotherapy allows the physiotherapist to be aware of all the factors that influence the patient’s state of health. In addition, it allows laying the foundations of pain neuroscience education
- The psychosocial factors the patient deals with can mean the intervention of other health professionals besides the physiotherapist ie important to take into account the professional limits, as well as the ethical principles that ensure the comprehensive management of the patient.
Criticisms of the model
- There is still minimal use of the biopsychosocial model in education, clinical care, and research. The biopsychosocial model cannot be consistently defined for an individual (data is not obtained systematically, making it untestable and non-scientific).
- Patient centered interview methods have been suggested to be used in practice, such that clinicians can identify a scientific BPS model specific to each patient with an agreed-upon, evidence-based patient-centered interviewing method can be more useful as these are reproducible and can elicit relevant patient information.[6]
Additional Resource
This article edited from an article produced by https://www.physio-pedia.com/Biopsychosocial_Model
Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiotherapy theory and practice. 2016 Jul 3;32(5):368-84